Strive Health's $550 million funding round shows how much investors love the idea of using AI to cut healthcare costs - NEA led the $300 million equity round while Hercules Capital threw in $250 million debt. But "value-based healthcare" often means "deny care to hit financial targets," and when you add AI to that equation, you get algorithmic rationing that could kill people.
The Kidney Care Crisis Gets the Silicon Valley Treatment
Chronic kidney disease hits 1 in 7 Americans, and 360 people start dialysis daily because the disease progresses silently until kidneys are severely damaged. It's a massive healthcare problem that actually needs solving.
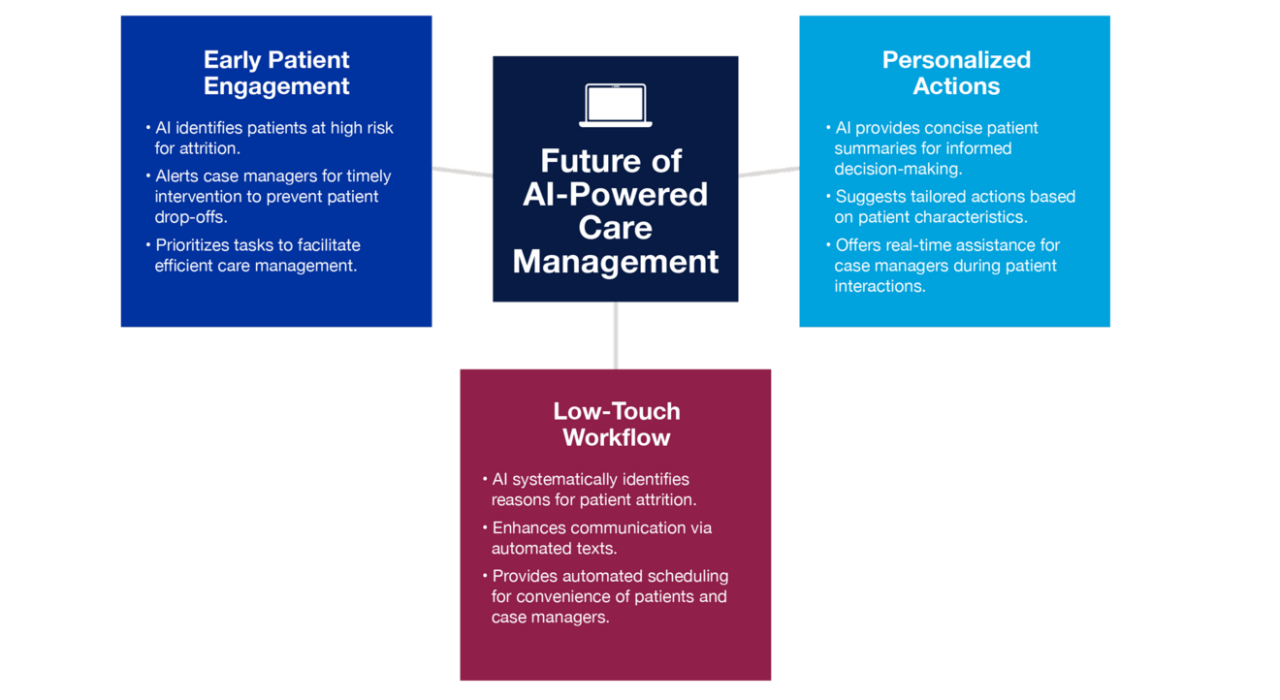
Strive's pitch sounds reasonable: catch kidney disease early, coordinate care better, and keep people out of dialysis centers. They manage 145,000 patients and $5 billion in medical spending across all states. But when you dig into "AI-powered care decisions," it often means algorithmic gatekeeping disguised as personalized medicine.
The Metrics That Matter (And The Ones They Don't Mention)
Strive claims 20% cost reductions and 41% fewer hospitalizations, which sounds great until you ask "what got cut to achieve those savings?" Did they catch kidney disease earlier, or did they delay expensive treatments until patients got sicker? Healthcare cost reduction often means care delay until it's too late to help.
The five-fold improvement in preemptive transplants is genuinely impressive - getting kidney transplants before patients need dialysis is clinically better and cheaper. But that metric works because it aligns financial incentives with patient outcomes. The scary part is when AI-driven cost optimization conflicts with patient needs.
CEO Chris Riopelle says they "integrate into the physician community" and partner with 700 nephrologists. That could mean "we help doctors provide better care" or "we use financial pressure to make doctors follow our protocols." In value-based care, the difference matters.
The "Kidney Hero" Marketing Bullshit
Central to Strive's success is their so-called "kidney hero care team" model, which pairs patients with dedicated care teams for continuous support between specialist visits. Led by nurse practitioners, these teams include case managers, care coordinators, social workers, dietitians, and pharmacists who coordinate care.
"This team is responsible for a patient and are coordinating and activating care," Riopelle explained. "We're not the cardiologist, but we're making sure they go to the cardiologist and they follow up with the treatment plan".
This approach addresses a critical gap in specialty care coordination, preventing patients from relying on emergency departments for routine management of their chronic conditions.
Strategic Investor Backing
The Series D round attracted significant institutional investment beyond lead investor NEA. CVS Health Ventures, CapitalG, Echo Health Ventures, Town Hall Ventures, and Redpoint joined the round, along with several new investors including funds managed by BlackRock affiliates.
Many of these same investors backed Strive's previous $166 million Series C round in 2023, indicating continued confidence in the company's growth trajectory and market opportunity. The repeat investment from strategic healthcare players like CVS Health Ventures demonstrates validation of Strive's approach to value-based specialty care.